- Inflammation, Negative Emotions, Mental Health
The role of inflammation in negative emotional states and mental disorders.

Author: Dr. Andréa Fuzimoto
Disclosure: This site contains links to our store. Some others may be affiliate links by which we may earn a small commission when you purchase certain products or services. This does not affect the prices that you may pay for them. By purchasing from us you help support this website and our services. Thank you!
The significant correlation between inflammation and negative emotions or mental disorders points to the importance of “emotional” management therapies in chronic inflammatory conditions.
Negative emotional states can engender inflammation, and inflammation may lead to a continuing generation of negative emotions. Inflammation is a process in which white blood cells, proteins, and fluids are driven to the site of injury to eliminate pathogens and repair tissues. This can create a lot of heat, congestion, and pain. These physiological changes can affect emotional and mental status. On the other hand, negative emotional states can also produce considerable heat and stagnation in the internal organ systems.
For people with chronic conditions and ongoing systemic inflammation, working on clearing heat and the stagnation caused by the inflammation is essential to improving emotional status. At the same time, “clearing” the negative emotional patterns can also help dissipate heat and reduce inflammation. Holistic and Traditional Medicines have different resources for reducing excessive inflammation which can damage tissues and for “clearing” negative emotional patterns. Interestingly, aspects of the relationship between inflammation and negative emotions or mental disorders have been evidenced by biomedical researchers in several peer-reviewed articles.
The inflammation and mental disorders connection
People with a history of early life stress and traumatic events may exhibit higher inflammatory markers leading to the development of PTSD and elevated rates of depression in adults.1 As part of this scenario, different factors may also play a role in triggering and/or worsening systemic inflammation such as inflammatory diet, gastro-intestinal permeability, changes in gut microbiota, obesity, smoking, sleep impairment, genetic inflammatory susceptibility, medical illnesses, infections, and psychological stress and/or trauma.1
As a consequence, systemic inflammation may trigger brain inflammation by trafficking peripheral immune cells and cytokines involved in the inflammatory process into the brain.1 Next, the central nervous system (CNS) inflammation may affect the reward circuitry leading to a reduction of dopamine and an increase of glutamate. Dopamine is a neurotransmitter that modulates learning and motivation.3 Dopamine deficiency causes anhedonia (loss of feeling of pleasure), a common finding in addiction and neuropsychiatric disorders. Glutamate is an excitatory neurotransmitter, and studies link an abnormal glutamate function to mood, anxiety, and trauma-related disorders such as PTSD.4
All this information shows how peripheral and CNS inflammation can affect our mental health and drive mood and anxiety disorders. However, biomedical science has not come to a definitive conclusion if anti-inflammatory drugs should be used as an alternative or adjuvant treatment for mental disorders. For Holistic Integrative Medicine (HIM), evaluating the presence and intensity of systemic and CNS inflammation is essential to treating mental disorders.
Biomedical research on inflammation and negative emotions
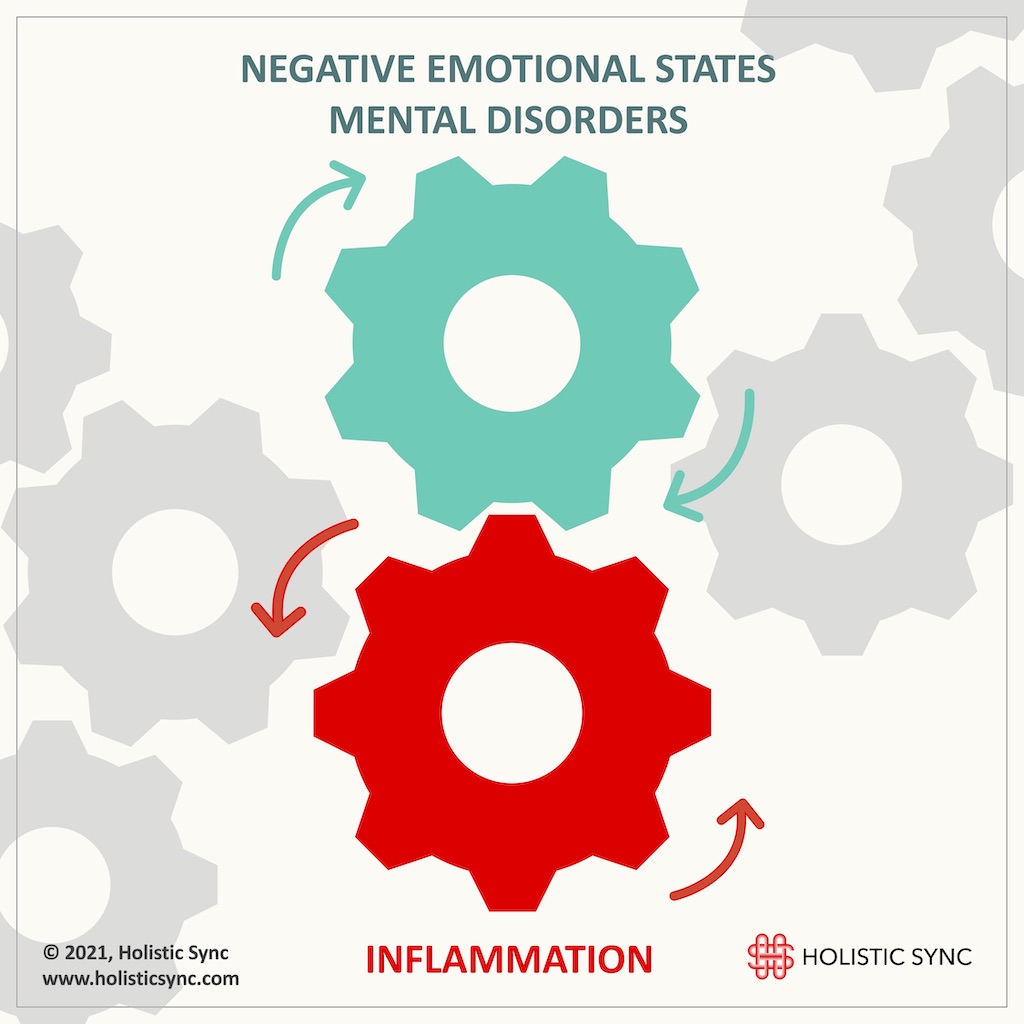
In a recent study (2019), researchers investigated the influence of negative emotions such as anger and sadness on the inflammatory markers interleukin-6 (IL-6) and C-reactive protein (CRP) of 226 adults.5 They concluded that anger predicted higher levels of IL-6 and chronic illnesses in old age.5 Likewise, anxiety, hostility, and fear were also linked to a higher IL-6 activity.6,7 Anxiety not only induced a significant increase in inflammatory cytokines but also in coagulant markers in cardiovascular disease-free people.8,9
Another research reported how anger can manifest in the inflammatory physiology of African Americans who showed a higher anger-out reaction, IL-6, and fibrinogen.10 Studies also examined the relationship between anger and the inflammatory marker and adhesion molecule sICAM-1, anger subdimensions (e.g. anger temperament, and anger reactions), and cynical hostility in 294 Mexican-American women. The results disclosed that cynical hostility was significantly associated with sICAM-1A and anger reaction was marginally associated with it.11 Since sICAM-1 is related to the risk of coronary vascular disease (CVD), anger and cynical hostility may predispose to CVD.11
Also, an experiment with a self-blame group expressing shame and guilt revealed a rise in the levels of tumor necrosis factor a receptors (sTNFaRII) demonstrating pro-inflammatory activity.12 Cleary, these studies demonstrate a connection between negative emotions and inflammation.
Studies show that negative emotional states increase inflammatory markers while positive emotional patterns are associated with lower inflammation markers.
On the other hand, people that cultivate more positive emotions seem to have less inflammation and may not be as much predisposed to developing chronic diseases.
One study linked happiness, excitement, and contentment to reduced levels of IL-6 and C-reactive protein (CRP) in women.13 In a different study, the researchers measured the inflammatory markers of 160 volunteers in perceived high-happiness and low-happiness groups. They also recruited 7 romantic couples and measured the inflammatory cytokines after warm physical contact with their partners. The results indicated that interferon-g (IFN-g) which can induce depression presented lower levels in the high-happiness group.14 This study demonstrated a correlation between the perception of happiness and inflammation, and that happiness may suppress the circulation of inflammatory cytokines.14
Another group of scientists evidenced that awe, wonder, and amazement which are associated with curiosity, desire to explore, and feeling of more social interconnectivity were linked to lower levels of pro-inflammatory cytokines such as IL-6.15 Researchers also showed that happier people with type 2 diabetes have lower inflammatory markers and a reduced basal IL-6 which was maintained after daily control of sadness.16 Thus, positive emotions seem to be related to lower levels of inflammation and chronic diseases.
Thus, negative emotions or mental disorders promote inflammation, and the cultivation of more optimistic and uplifting emotional patterns can greatly influence our immune system and counteract inflammation. This correlation shows the importance of supportive “emotional” therapies in chronic conditions. The cultivation of happiness and positive emotional patterns may be the most important factor in the recovery of chronic diseases.

Dr. Andréa Fuzimoto, DAOM, MSTCM, MSCS, CSAS, Dipl. O.M (NCCAOM®/USA), L.Ac. (CA/USA); PT/Acu (BR) is a clinician and researcher working with Holistic Integrative Medicine (HIM) with emphasis in gastrointestinal, neurological, and immunological conditions. Patients look for her careful diagnostic evaluation, strategic treatment planning, and compassionate care. As a researcher, she is a peer-reviewed published author and a Elsevier certified peer-reviewer contributing to different scientific journals. She has trained and worked in centers of excellence such as the Stanford University Medical School (Pain Medicine Division) with NIH-funded Clinical Trials, and the California Pacific Medical Center (CPMC), at the Stroke Clinic, among others. For more information on her specialties and certifications, visit Linkedin.
References
- Felger J. Imaging the Role of Inflammation in Mood and Anxiety-related Disorders. Curr Neuropharmacol. 2018;(16(5):533-558). doi:https://doi.org/10.2174/1570159×15666171123201142
- Michopoulos V, Rothbaum A, Jovanovic T, et al. Association of CRP Genetic Variation and CRP Level With Elevated PTSD Symptoms and Physiological Responses in a Civilian Population With High Levels of Trauma. Am J Psychiatry. 2015;(172(4):353-62). doi:10.1176/appi.ajp.2014.14020263
- Berke J. What Does Dopamine Mean? Nat Neurosci. 2018;(21(6):787-793). doi:10.1038/s41593-018-0152-y
- Averill L, Purohit P, Averill C, Boesl M, Krystal J, Abdallah C. Glutamate Dysregulation and Glutamatergic Therapeutics for PTSD: Evidence From Human Studies. Neurosci Lett. 2017;(649:147-155). doi:10.1016/j.neulet.2016.11.064
- Barlow M, Wrosch C, Gouin J, Kunzmann U. Is Anger, but Not Sadness, Associated With Chronic Inflammation and Illness in Older Adulthood? Psychol Aging. 2019;(34(3):330-340). doi:10.1037/pag0000348
- Suarez A. Joint Effect of Hostility and Severity of Depressive Symptoms on Plasma Interleukin-6 Concentration. Psychosom Med. 2003;(65(4):423-7). doi:10.1097/01.psy.0000062530.94551.ea
- Moons W, Eisenberger N, Taylor S. Anger and fear responses to stress have different biological profiles. Brain Behav Immun. 2010;(24(2):215-9). doi:10.1016/j.bbi.2009.08.009
- Moons W, Shields G. Anxiety, Not Anger, Induces Inflammatory Activity: An Avoidance/Approach Model of Immune System Activation. Emotion. 2015;(15(4):463-76). doi:10.1037/emo0000055.
- Pitsavos C, Panagiotakos D, Papageorgiou C, Tsetsekou E, Soldatos C, Stefanadis C. Anxiety in relation to inflammation and coagulation markers, among healthy adults: The ATTICA Study. Atherosclerosis. 2006;(185(2):320-6). doi:10.1016/j.atherosclerosis.2005.06.001
- Boylan J, Lewis T, Coe C, Ryff C. Educational Status, Anger, and Inflammation in the MIDUS National Sample: Does Race Matter? Ann Behav Med. 2015;(49(4):570-8). doi:10.1007/s12160-015-9687-2
- Shivpuri S, Gallo L, Mills P, Matthews K, Elder J, Talavera G. Trait Anger, Cynical Hostility and Inflammation in Latinas: Variations by Anger Type? Brain Behav Immun. 2011;(25(6):1256-63). doi:10.1016/j.bbi.2011.04.016
- Dickerson S, Kemeny M, Aziz N, Kim K, Fahey J. Immunological Effects of Induced Shame and Guilt. Psychosom Med. 2004;(66(1):124-31). doi:10.1097/01.psy.0000097338.75454.29
- Steptoe A, O’Donnell K, Badrick E, Kumari M, Marmot M. Neuroendocrine and Inflammatory Factors Associated with Positive Affect in Healthy Men and Women. Am J Epidemiol. 2008;(167(1):96-102). doi:10.1093/aje/kwm252
- Matsunaga M, Isowa T, Yamakawa K, et al. Association Between Perceived Happiness Levels and Peripheral Circulating Pro-Inflammatory Cytokine Levels in Middle-Aged Adults in Japan. Neuro Endocrinol Lett. 2011;(32(4):458-63).
- Stellar J, John-Henderson N, Anderson C, Gordon A, McNeil G, Keltner D. Positive Affect and Markers of Inflammation: Discrete Positive Emotions Predict Lower Levels of Inflammatory Cytokines. Emotion. 2015;(15(2):129-33). doi:10.1037/emo0000033
- Panagi L, Poole L, Hackett R, Steptoe A. Happiness and Inflammatory Responses to Acute Stress in People With Type 2 Diabetes. Ann Behav Med. 2019;(53(4):309-320). doi:10.1093%2Fabm%2Fkay039