- Probiotics, Prebiotics, Symbiotics, Postbiotics, Paraprobiotics, Microbiota, Microbiome, Dysbiosis, Gut Health, Chronic Diseases
The evolution of the probiotics and microbiota-microbiome-related therapies.

Author: Dr. Andréa Fuzimoto
Disclosure: This site contains links to our stores. Some others may be affiliate links by which we may earn a small commission when you purchase certain products or services. This does not affect the prices that you may pay for them. By purchasing from us you help support this website and our services. Thank you!
The probiotics or “for life” products have a long history as nutritional and therapeutic foods dating back 10,000 years.1 The traditional fermented products such as beer, bread, wine, kefir, kumis, and cheese are the foundations of a renewed modern medical approach of using microorganisms to modulating the neuroendocrine-immune systems to prevent and treat diseases. This has culminated in the development of probiotics, prebiotics, symbiotics, postbiotics, and paraprobiotics.
Our story of fermented foods starts with fermented milk in the Middle East (10,000 BCE), in Egypt, Greece, and Italy (7,000-5,000 BCE).2

The Egyptians, Phoenicians, and Eastern cultures stored the milk of cows, sheep, goats, horses, and camels in bags made from the skin or the stomach of these same animals.2 There, the milk was in contact with the animals’ microorganisms, went through a fermentation process transforming it into a thick and creamy custard.2 This process associated with the low humidity and a hot climate, created the yogurt. Considered by the Turks as the “elixir of life”, the word yogurt comes from the verb “yoğuşmak” which means thicken or curdle.2 The Turks used yogurt to prevent or treat gastrointestinal problems.1 Yogurt and products made from fermented milk are considered the first functional foods.2
In the 16th century, the French King, Francis I, suffered from a severe gastrointestinal disease. Upon requesting assistance from Suleiman, the Magnificent, an Ottoman doctor was sent to treat him. He provided a successful treatment through the use of yogurt.1 The Roman army commander, writer, and philosopher Pliny the Elder (23-79 CE) wrote an encyclopedia entitled “Naturalis Historia” in which he described fermented milk as a treatment for diarrhea and vaginal discharge.1 Also, Genghis Khan added fermented milk to the list of provisions of his army as it was an easy way to provide nutrition in a preserved form.1 However, milk was not the only fermented product that was developed in antiquity. Other examples are the beer produced from malted cereals, wine, tea, soy sauce, bread, fish sauce, garum (from fish guts), pickled vegetables, and fermented rice, mushrooms, and honey (mead).2
Fermented beverages were being produced as early as the Neolithic age. In an archeological excavation in the village of Jiahu (Henan province, China), the analysis of the pottery jars revealed a fermented beverage made of rice, honey, and fruits (hawthorn fruit and/or grape) dated from 6,000 BCE.3 For the ancient Chinese culture, these beverages had social, religious, and medical significance.3 During the pre-Hippocrates period, wine was used as an antiseptic, anesthetic, sedative, hypnotic, appetite stimulant, anti-convulsive, diuretic, purgative, anti-diarrheal, antipyretic, and anti-anemic.1 In the 14th century, the Catalan physician and scientist, Arnaldus de Villa Nova recommended wine for dementia, sinus disorders, and other conditions.1 In 1790, the first paper on a scientific journal describing a combination of wine and medicines for rickets and dysentery was published.1
Interestingly, the probiotic therapies extended beyond their consumption in food forms. The first medical record of fecal transplant as a means of transferring probiotics from one person to another was described by Ge Hong (283-343 CE), a famous physician and philosopher from the Eastern Jin dynasty in China.2 He recommended an orally administered fecal preparation for food poisoning and severe diarrhea. Also, in Africa, the Bedouins ingested fresh camel feces to treat dysentery, and the active ingredient was later identified as Bacillus subtilis.2 Nowadays, the use of fecal transplant is being researched and used for hard-to-treat conditions such as C. difficile infection related to antibiotic-associated diarrhea (AAD). For most of its history, the medical knowledge on the beneficial probiotics and fermented foods was empirical. It was not until much later that the science of microbiology was developed and the first bacteria and yeast were uncovered.
Modern history and the foundation of the science of probiotics
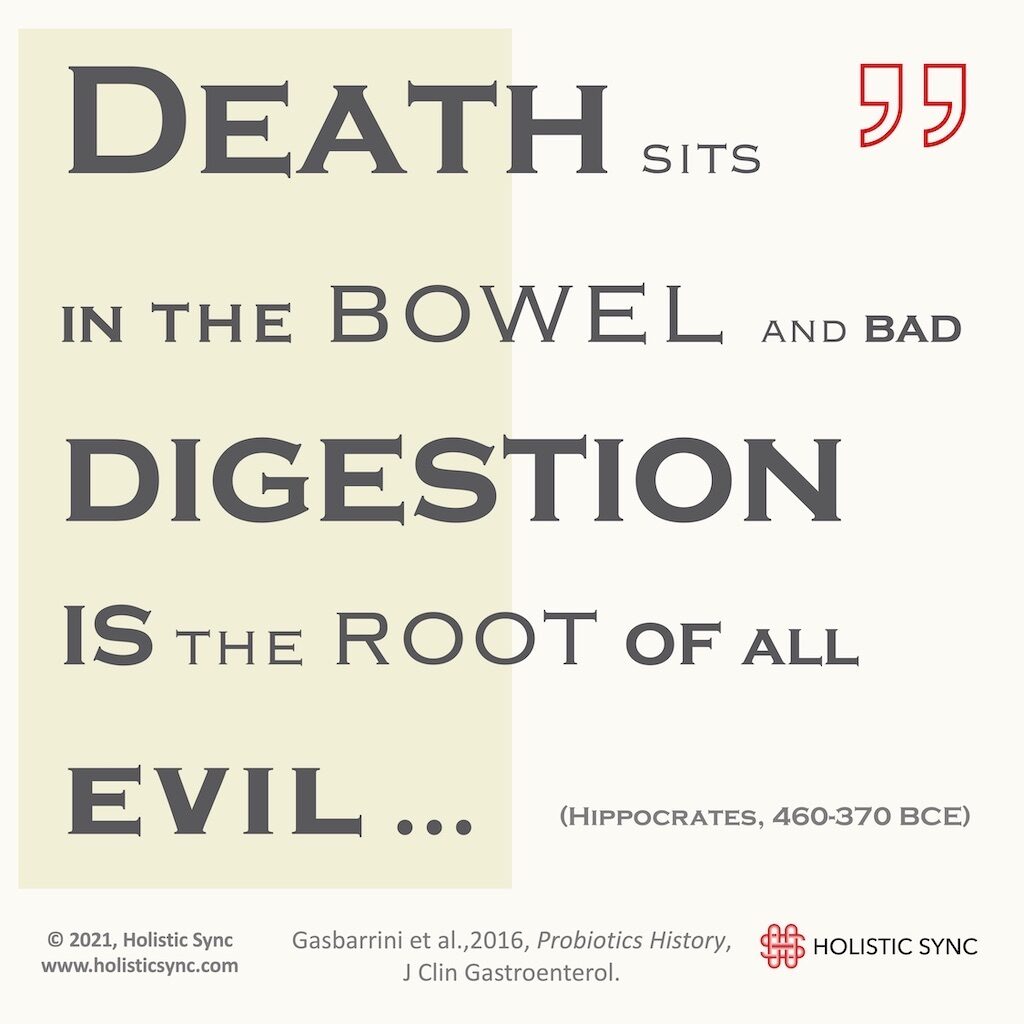
There are two types of fermentation. Yeast produces alcoholic fermentation, and bacteria yield lactic acid fermentation. In 1857, Louis Pasteur (1822-1895 CE) discovered the lactic acid-producing bacteria, and he was the first to experimentally demonstrate the fermentation process.1,2 In 1889, Henry Tissier, a pediatrician of the Pasteur Institute uncovered the Bifidobacterium spp.1 Tissier was the first scientist to defend the idea that good bacteria such as Bifidobacterium could balance the harmful bacteria and resolve diseases such as gastroenteritis.1 In 1917, a German Professor, Alfred Nissle discovered a non-pathogenic bacterium named Escherichia coli Nissle strain which inhibits the adherence of pathogenic bacteria.1 Then, a Bulgarian physician, Stamen Grigorov (1878-1945), identified a Lactobacillus present in the kisselo mliako, the Bulgarian yogurt.1 Grigorov was invited by the renowned scientist Elie Metchnikov to visit the Pasteur Institute and give a lecture when he successfully demonstrated the existence of the lactic acid-producing L. bulgaricus. Metchnikov went on to concentrate his studies on these probiotics, and on the hypothesis that the villagers in Bulgaria lived longer because of fermented milk health effects.1 He suggested that the Lactobacilli counteracted the putrefactive effects of the gastrointestinal metabolism which contributed to illness and aging. Elie Metchnikov ended up being awarded the Nobel Prize in Physiology and Medicine (1908) in recognition of his work in immunology.
The use of probiotic-containing foods would modify the flora, replace the harmful microbes, and promote health and longevity. Metchnikov caused a propulsion of the yogurt industry in France which then spread to other parts of the world.2 In 1930, Dr. Minoru Shirota from Medicine Kyoto University in Japan isolated for the first time the Lactobacillus casei Shirota strain from the human intestine.1 These probiotics were used to create the yakult, the drink named after the word yogurt in Esperanto. Finally, in 1953, the word “probiotics” was first introduced by the German scientist Werner Kollath as “active substances that are essential for a healthy development of life”.2 Since then, the research on the intestinal flora caused another wave of discoveries and revealed how these microorganisms can impact health and diseases.
The evolution of the probiotics and their biological properties
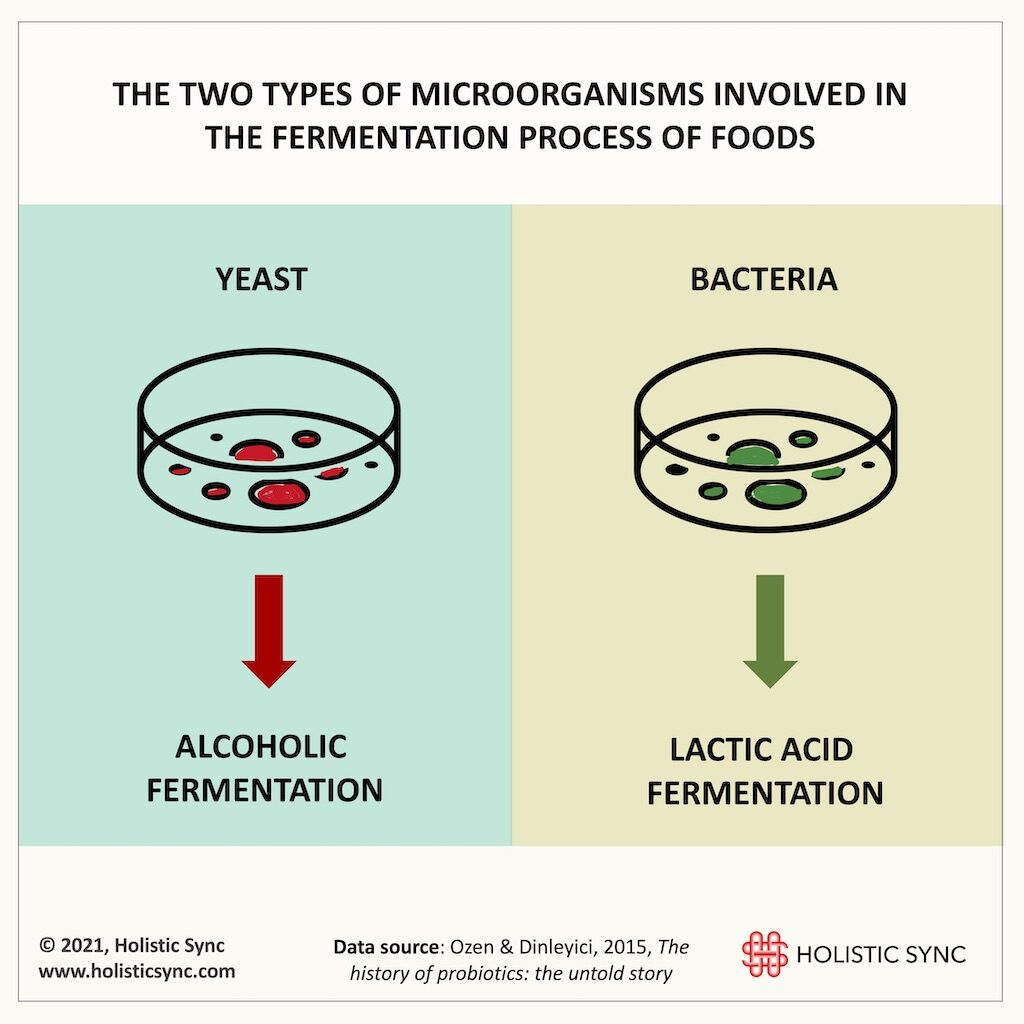
Probiotics are “live organisms that when administered in adequate amounts confer health benefits to the host”.4 The probiotics supply microorganisms to the gastrointestinal tract, and promote digestion and absorption of foods, reduce pathogenic flora, maintain intestinal barrier integrity, and modulate the immune system.5 The World Health Organization (WHO) categorized four (4) products that contain live organisms, three of them are considered dietary supplements, and one is considered a drug. These four are:
1. the foods that contain active cultures;
2. the foods and supplements that have probiotics with no health claim;
3. the foods and supplements with probiotics with a specific health claim:
4. the probiotic drugs that are used to treat and prevent diseases.4
The biological properties attributed to probiotics include anti-microbial, antioxidative, anti-aging, anti-biofilm, anti-carcinogenic, anti-diabetic, anti-lactose intolerance, and enhancement of the immune system.6 On the other hand, prebiotic is defined as food that stimulates the growth and/or activity of intestinal bacteria. The main prebiotics that promote the proliferation of the Lactobacillus and the Bifidobacterium are the fructo-oligosaccharides and galacto-oligosaccharides. Prebiotics are typically carbohydrate polymers that are not digested nor absorbed by the human intestines.4 However, scientists also proposed that non-carbohydrates can act as prebiotics such as resistant starch, pectin, arabinoxylan, whole grains, various dietary fibers, and non-carbohydrates that can act through gut microbiota modulation.4 Other examples of prebiotics include human milk oligosaccharides (HMO), lactulose, and inulin derivatives.5
The combination of probiotics and prebiotics is called symbiotics, and it intends to increase the growth of probiotics and augment their health benefits.4 Recently, another concept arouse, the postbiotics. The postbiotics do not contain live organisms and are metabolites released or produced by the activity of the intestinal microorganisms which directly or indirectly exert health benefits to the host.5 They include cell-free supernatants, exopolysaccharides, enzymes, short-chain fatty acids (SCFA), bacterial lysates, vitamins, and amino acids, to cite a few.5 Collectively, postbiotics exhibit anti-inflammatory, anti-oxidant, anti-tumor, and antimicrobial properties, modulate the immune system by restoring the balance between Th1/Th2 cells, normalize intestinal peristalsis, positively influence intestinal barrier, stabilize blood glucose, and possess “statin-like” activity.5 The microbiota can be regulated by the use of probiotics, prebiotics, symbiotics, and postbiotics.5 Although studies show good results of the probiotics for the treatment of several diseases, some researchers point to the risk of using live organisms when there is an increased permeability of the gut lining or in children with an immature immune system.5 Concerning that, prebiotics and postbiotics have no side effects while delivering similar benefits of the probiotics.5
Yet, another development came in the form of the paraprobiotics. The paraprobiotics, also called “ghost or inactivated” probiotics, are intact or broken inactivated or dead microbial cells that when administered in adequate amounts provide health benefits.6 Some examples of paraprobiotics are teichoic acid, peptidoglycan, cell-wall polysaccharides, cell-surface associated proteins, and proteinaceous filaments. The “death” of the probiotics is achieved by heat, gamma or ultraviolet irradiation, chemical treatment, and other techniques. Importantly, these “dead” cells maintain their potential to provide favorable properties in the host’s intestine. Interestingly, research is showing that the heat-killed probiotics have a similar mode of action to the live probiotics.6 Some of the properties of the paraprobiotics consist of anti-inflammatory, anti-oxidative, anti-intestinal barrier disruption, anti-biofilm, immune-modulatory, and anti-adhesion of pathogenic organisms.6 So, the use of metabolites of dead cells of probiotics is the new frontier in the microbiota-microbiome-related therapies to address medical conditions. Despite the considerable recent scientific developments in this field, it seems that there is a lot more to be uncovered in this fertile area of research to address a wide range of diseases.
The use of probiotics-related therapies for diseases
In recent years, science has been uncovering the relationship between the gut commensal and pathogenic microorganisms and the intestinal immune and nervous systems. Dysbiosis is an imbalance of these intestinal organisms (microbiota), and studies show that it may lead to the development of autoimmune diseases (e.g. inflammatory bowel disease, type 1 diabetes), cancer, psychiatric problems, and other ailments.5 Evidence supports that obesity and its metabolic effects are strongly related to both the composition and function of the microbiota.7 Supplementation of Lactobacillus, Bifidobacterium, Saccharomyces, Streptococcus, and Enterococcus may play a role in the prevention and management of obesity.7 Many other species have and are being studied. Apart from regulating the host metabolic functions, the gut microbiota also dampens chronic inflammation which is also present in obesity. Furthermore, prebiotics showed beneficial effects against obesity through different mechanisms of action.7 Nonetheless, the role of probiotics and prebiotics in the improvement of diseases is controversial and a lot more research is necessary to determine the microbiota-microbiome patterns or signatures of different diseases to inform effective therapeutic approaches.
The changes in the composition and activity of the intestinal microbiota after the ingestion of probiotics-prebiotics alter the gene expression pattern (transcriptomics) and metabolism (metabolomics) of the host.8 This is another way probiotics, prebiotics, and symbiotics could be used to modulate the immune and nervous systems of people with medical conditions. Studies revealed promising results of probiotics and prebiotics for autism spectrum diseases (ASD) and cancer.8 The combination of the probiotic VLS#3 and E. coli Nissle 1917 demonstrated beneficial results for ulcerative colitis (UC). Also, similar beneficial effects for UC were achieved by the symbiotic association of Bifidobacterium bevere and galacto-oligosaccharide, and Bifidobacterium longum mixed with inulinoligofructose.8 A relationship between gut dysbiosis and non-alcoholic fatty liver (NAFL) was proposed and probiotics/symbiotics are being investigated as a supportive treatment for NAFL.9 Generally speaking, any diseases that are linked to dysbiosis may benefit from the use of probiotic therapies to balance the gut microorganisms. Some examples are Parkinson’s disease, Inflammatory bowel diseases (Crohn’s disease and ulcerative colitis), and autoimmune diseases such as type 1 diabetes, multiple sclerosis (MS), rheumatoid arthritis (RA), and systemic lupus erythematosus (SLE), to cite a few.10,11,12 On another note, the postbiotic metabolites from the six species of Lactobacillus plantarum caused cell death in various cancer cells while sparing the normal cells and with no toxic effects.13 Probiotics and paraprobiotics were proposed as remedies for the prevention and treatment of several viral infections.14 The postbiotics and paraprobiotics stand for natural antibiotic alternatives with potential future clinical applications.
Hippocrates (460-370 BCE) had already pointed out that ”death sits in the bowel” and that “bad digestion is the root of all evil” thus emphasizing the importance of gastrointestinal health.2 Ancient physicians thought animal milk was not adequate food for humans, and Hippocrates and Galeno recommended it only for medicinal use.2 The Romans, for example, were the first to use cow milk which was considered harmful, instead of sheep milk.2 The idea of milk and fermented products were already seen as remedies. The current scientific articles seem to agree with this notion. Although probiotics and related products are considered of low risk, some studies warrant caution when using with immunocompromised patients, in multiple organ failure, malnourished patients, cancers, leaky gut, and in children with an immature immune system.8 While many diseases showed the presence of dysbiosis and could benefit from the use of probiotics and related therapies, we still don’t know the patterns and/or signatures of the microbiota-microbiome in specific diseases. The functions of each species of probiotics vary significantly and thus may influence the health of patients in different ways. Lab testing for the flora composition may be a good first step to understanding the individual intestinal health status to devise an individual treatment plan.

Dr. Andréa Fuzimoto, DAOM, MSTCM, MSCS, CSAS, Dipl. O.M (NCCAOM®/USA), L.Ac. (CA/USA); PT/Acu (BR) is a clinician and researcher working with Holistic Integrative Medicine (HIM) with emphasis in gastrointestinal, neurological, and immunological conditions. Patients look for her careful diagnostic evaluation, strategic treatment planning, and compassionate care. As a researcher, she is a peer-reviewed published author and a certified peer-reviewer contributing to different scientific journals. She has trained and worked in centers of excellence such as the Stanford University Medical School (Pain Medicine Division) with NIH-funded Clinical Trials, and the California Pacific Medical Center (CPMC), at the Stroke Clinic, among others. For more information on her specialties and certifications, visit Linkedin.
References
- Ozen M, Dinleyici E. The history of probiotics: the untold story. Benef Microbes. 2015;(6(2):159-65). doi:https://doi.org/10.3920/bm2014.0103
- Gasbarrini G, Bonvicini F, Gramenzi A. Probiotics History. J Clin Gastroenterol. 2016;(Suppl 2, Proceedings from the 8th Probiotics, Prebiotics&New Foods for Microbiota and Human Health meeting held in Rome, Italy on September 13-15, 2015:S116-S119.). doi:https://doi.org/10.1097/mcg.0000000000000697
- McGovern P, Zhang J, Tang J, et al. Fermented beverages of pre- and proto-historic China. Proc Natl Acad Sci USA. 2004;(101(51):17593-17598). doi:https://dx.doi.org/10.1073%2Fpnas.0407921102
- Quigley E. Prebiotics and Probiotics in Digestive Health. Clin Gastroenterol Hepatol. 2019;(17(2):333-344). doi:https://doi.org/10.1016/j.cgh.2018.09.028
- Zolkiewicz J, Marzec A, Ruszczynski M, Feleszko W. Postbiotics-A Step Beyond Pre- and Probiotics. Nutrients. 2020;(12(8):2189). doi:https://doi.org/10.3390/nu12082189
- Nataraj B, Ali S, Behare P, Yadav H. Postbiotics-parabiotics: the new horizons in microbial biotherapy and functional foods. Microb Cell Fact. 2020;(19(1):168). doi:https://doi.org/10.1186/s12934-020-01426-w
- Cerdó T, García-Santos J, Bermúdez M, Campoy C. The Role of Probiotics and Prebiotics in the Prevention and Treatment of Obesity. Nutrients. 2019;(11(3):635). doi:https://doi.org/10.3390/nu11030635
- Tsai Y, Lin T, Chang C, et al. Probiotics, prebiotics and amelioration of diseases. J Biomed Sci. 2019;(26(1):3). doi:https://doi.org/10.1186/s12929-018-0493-6
- Xie C, Halegoua-DeMarzio D. Role of Probiotics in Non-alcoholic Fatty Liver Disease: Does Gut Microbiota Matter? Nutrients. 2019;(11(11):2837). doi:https://doi.org/10.3390/nu11112837
- Sun M, Shen Y. Dysbiosis of gut microbiota and microbial metabolites in Parkinson’s Disease. Ageing Res Rev. 2018;(45:53-61). doi:https://doi.org/10.1016/j.arr.2018.04.004
- Yu L. Microbiota dysbiosis and barrier dysfunction in inflammatory bowel disease and colorectal cancers: exploring a common ground hypothesis. J Biomed Sci. 2018;(25(1):79). doi:https://doi.org/10.1186/s12929-018-0483-8
- Oliveira G, Leite A, Higuchi B, Gonzaga M, Mariano V. Intestinal dysbiosis and probiotic applications in autoimmune diseases. Immunology. 2017;(152(1):1-12). doi:https://doi.org/10.1111/imm.12765
- Chuah L, Foo H, Loh T, et al. Postbiotic metabolites produced by Lactobacillus plantarum strains exert selective cytotoxicity effects on cancer cells. BMC Compelment Altern Med. 2019;(19(1):114). doi:https://doi.org/10.1186/s12906-019-2528-2
- Kanauchi O, Andoh A, AbuBakar S, Yamamoto N. Probiotics and Paraprobiotics in Viral Infection: Clinical Application and Effects on the Innate and Acquired Immune Systems. Curr Pharm Des. 2018;(24(6):710-717). doi:https://doi.org/10.2174/1381612824666180116163411